Prologue: What follows is a look at the use of 68Gallium as part of a positron emitting radioligand from an organometallic chemist’s point of view. I’m not from nuclear medicine nor am I a radiation oncologist.
It had to happen … the other shoe has dropped. My stage-4 prostate cancer has come charging back for round 2 after 9 years. Again, I’ve taken a personal interest in radiation oncology. Recently, my PSA shot up steeply through the 4.0 ng/dL threshold triggering an appointment with my radiation oncologist who has ordered a PET/CT scan. Back in 2015 I finished 18 months of hormone ablation (chemical castration) and got the PSA from 29 down to 0.01 with Lupron injections and earlier, a large cumulative dose of x-radiation in the lower abdomen. I have to say that while I experienced no discomfort at all in this round of treatment, I did lose body hair and muscle mass.
PET/CT scanning is an important tool in locating prostate cancer cells. Riding the platform in and out of the scanner is expensive but important. Unfortunately for me, the CT contrast agent is a potent emetic so the scanner becomes an expensive vomitorium ride.
The story of PET, Positron Emission Tomography, has evolved over decades of advancement. To begin, tomography, detectors and computers had to be invented. Separately, positron emission as a medically viable radiation source had to be identified and validated. A substrate for selective delivery of the isotope must be found. In the case of 18Fluorine, it is available as an organofluorine molecule like 18F-Glucose. It turns out that the 18F-Glucose concentrates in clinically useful places and K18F does not.
Positron Emitters
Atomic nuclei that are deficient in neutrons can have an instability leading to emission of a positron (anti-electron with a + charge), also called a β+ decay, which lessens the neutron deficiency by ejecting a positive charge from the nucleus. When a positron is ejected from the nucleus it finds itself immediately swarmed by the electron clouds of surrounding atoms and molecules and doesn’t travel very far. When a positron encounters a negatron (regular electron, β−), they annihilate one another and emit two gamma photons of 511 keV energy at 180 degrees apart. This is a mass to energy conversion. Loss of one positive charge from the nucleus gives rise to a transmutation of the atom causing a one-unit drop in atomic number, that is it goes from n+ to (n – 1)+, but retains most of its atomic weight. In this case, 6831Gallium undergoes positron decay to 6830Zinc.
Positron emitters include 11Carbon (T1⁄2 = 20.4 min), 13nitrogen (T1⁄2 = 10 min), 15oxygen (T1⁄2 = 2 min), 18fluorine (T1⁄2 = 110 min), 64copper, 68gallium, 78bromine, 82rubidium, 86yttrium, 89zirconium, 22sodium, 26aluminium, 40potassium, 83strontium, and 124iodine. This a list given by Wikipedia, but there are many more in more comprehensive tables.
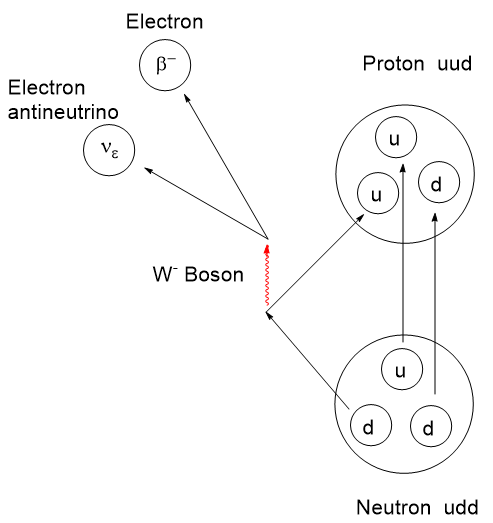
The actual mechanism of β-type emission requires a venture into fundamental particles called quarks. Protons and neutrons are composite particles called hadrons, not fundamental particles. Protons and neutrons are each comprised of 3 quarks, but with a different combination of “up and down flavors” where flavor refers to the species of quark. There are 6 flavors of quarks: up, down, charm, strange, top, and bottom. Interconversion between protons and neutrons can occur if one of the 3 top or bottom quarks changes flavor. By all means, if this interests you, take a dive into it. I shall stop here.
Positron emitters tend to have a short radioactive half-life as well as a limited chemical half-life in the body before they are cleared out through the kidneys or other routes. Ideally, the goal is to deliver a high radiation dose selectively to a target tissue as fast as is safe then disappear. Prolonged irradiation to surrounding tissue is undesirable. The optimal radiopharmaceutical will be highly target selective and have a short half-life. A selective radiopharmaceutical is one that will accumulate in a desired cell type or organ. Accumulation can be aided through simple solubility, the ability to undergo transport through a cell wall, affinity to a specific receptor and the ability to function fast enough to resist the various clearance mechanisms.
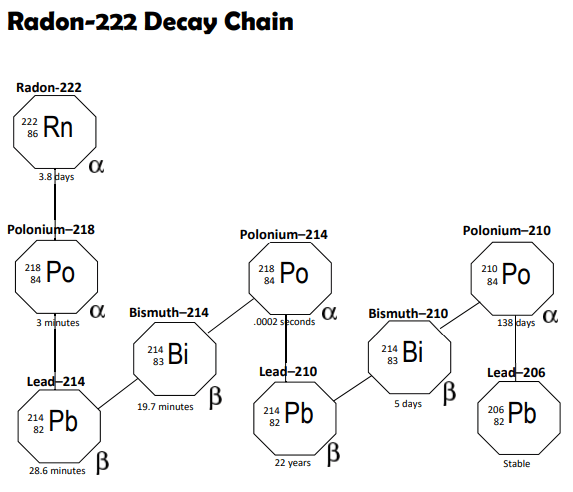
A short half-life means that the radioactivity per gram of radioisotope, specific activity in Becquerels per gram, will be at its maximum after activation. Though the radioactivity may be intense, the radiation dose can be controlled by the amount of mass administered. With radioisotopes, there are two kinds of purity to consider: Chemical purity referring to the atoms and molecules present; Radiological purity referring to the presence or absence of other radioactive isotopes. To provide maximum safety and effectiveness, the specific radioisotope with the desired decay mode should be the only source present. If your desired source is an alpha emitter, you don’t need spurious quantities of a gamma emitter present because of inadequate purification.
Economical methods of preparing positron emitters had to be addressed. To fully exploit PET for any given situation, tissue selectivity of radioligands had to be determined and selective positron radiopharmaceuticals developed. Due to the short half-life of these radioisotopes, rapid and safe methodologies to produce them by efficient nuclear transformations, isotope isolation followed by chemical synthesis had to be developed. It is important that isotope generation, isolation and attachment to a ligand be done nearby the hospital for the proper activity to reach the patient.
Positron emitter production involves a nuclear reactor for neutron activation or a cyclotron accelerating protons or deuterons in the preparation. Because both of these sources are highly destructive to organic molecules, an inorganic radioisotope is produced separately and chemically modified to produce an inorganic species that can be chelated or otherwise attached to a radiopharmaceutical. This technique evolved from simple radiography in the 1930’s to a large array of techniques and applications today. The reader is invited to take a dive into this topic.
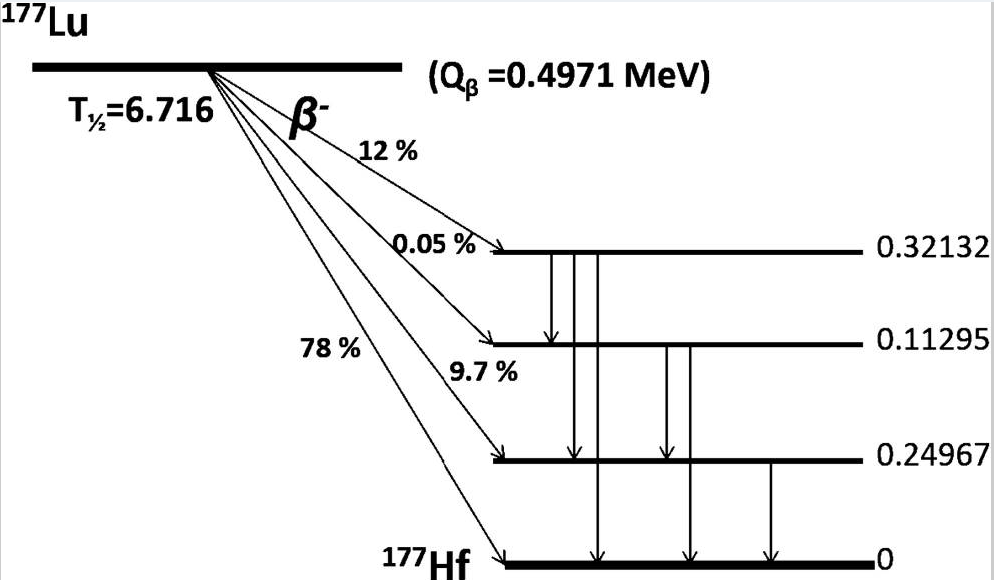
Since my cancer experience began, a few new radiotherapies and imaging agents have landed in oncology space for prostate cancer. Recently I posted on Pluvicto PSMA (Prostate Specific Membrane Antigen) which was before I knew about my current prostate situation. PSMA is a transmembrane protein present in prostatic cells. Pluvicto uses a chelated 177Lutetium beta emitter as the destructive warhead and a peptidomimetic fragment for binding to the PSMA receptor.
A Brief Interlude into Quality Factor
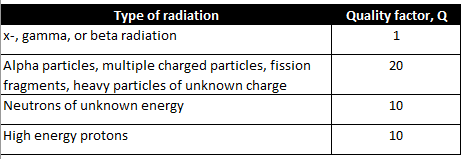
It should be noted that the various forms of particle (alpha, beta, or neutron) or electromagnetic radiation (x-ray or gamma) have differing abilities to penetrate and cause ionization of within matter. There is a factor for this which is used to refine dosage calculations. It is called the Quality factor, Q.
The destructive effects of radiation stem from its ability to ionize matter along its path. Ionization is a disruptive effect that may result in fragmentation of molecules or crystal lattices into reactive positive or negative ions. Single electron radical species may be formed as well. It is possible for some fraction of the disrupted molecules to recombine if the fragments haven’t already diffused away or gone on to further transformations.
The deleterious effects of radiation on living tissue stems from the amount of disruptive energy transferred to tissues along the path of each particle. Charged particles like electrons, protons and alpha particles tend to dump their energy into matter rapidly and along a short path making them less penetrating than neutrons or electromagnetic rays in general.
Quality factor, Q, is a dimensionless coefficient that is multiplied by an absorbed dose to give a more realistic estimation of radiation energy absorption. Interestingly, the Q for neutrons varies with energy and rises to a maximum around 0.5 to 1 MeV of energy and falls off at higher energies.
The larger the Q factor, the larger the corrected radiation effect. X-, gamma, and beta radiation have a Q factor lower than the others by a factor of 10 to 20. The x- and gamma rays will tend to pass through matter leaving a small amount of their energy to disruption. In radiation therapy this is compensated for by just increasing the fluence or the exposure time.
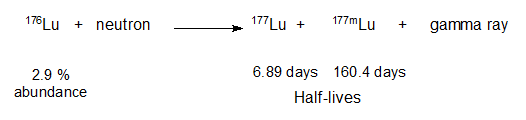
For clarity, x-rays are generated from the electron cloud around an atom via electron transitions. For instance, if an electron is dislodged from an inner, low energy orbital, another electron can occupy that vacancy by the emission of an x-ray. Gamma rays originate from nuclear energy transitions. Often a nuclear decay might result in a new nucleus that is not at its ground state and would be categorized as metastable. This metastable state, which has its own half-life, can collapse to its ground state by the emission of a gamma ray matching the loss of energy by the nucleus.
Neutrons
Free neutrons are special. They undergo beta decay with a short half-life outside the nucleus having t1/2 = ~ 10-15 minutes, depending on the information source. Not having a charge, they tend to be more penetrating than other particles. However, effective shielding can be had with a hydrocarbon like paraffin or water by virtue of the high concentration of hydrogen nuclei present in these substances. Neutrons are not affected by charge repulsion from an atomic nucleus and therefore can collide and interact with the hydrogen nucleus (a proton). They can scatter from hydrogen nuclei, leaving behind some of their kinetic energy with each collision (see “Neutron Lethargy“). This scattering is the basis for using water to moderate the neutrons in a nuclear reactor. Neutrons are cooled by repeated collisions with hydrogens in water to the point where their kinetic energy of 0.025 eV, which from the Maxwell-Boltzmann distribution corresponds to a temperature of 17 oC, thus the term “thermal neutrons“.
Many elements absorb neutrons, increasing the atomic weight and very often altering the stability of the nucleus leading to a radioactive decay cascade. This is what is happening in neutron activation. In the case of water, the ability of free neutrons to collide with hydrogen nuclei allows them to dislodge hydrogen ions or free radicals from organic and biomolecules resulting in ionization and makes them quite hazardous to living things.
Radioligands
Drugs like Pluvicto are referred to as a radioligand. There is a radioisotope connected to an organic “ligand” for selective binding to a specific protein receptor. A radioligand is injected and diffuses its way a particular receptor where it binds. As it turns out, due to the gamma radiation also emitted by 177Lu, Pluvicto is a radioligand that can also be located in the body by the gamma radiation it emits. In general, a radioligand can be used for two endpoints: To find and signal the location of a particular cell type; and to find and vigorously irradiate a particular cell type.
There are recent radioligand compounds that are used as PET (Positron Emission Tomography) diagnostic agents which selectively bind to the PSMA receptor where they can undergo positron emission revealing the site of prostate cancer cells by tomography. 18F-glucose was first synthesized in 1967 in Czechoslovakia at Charles University by Dr. Josef Pacák and was first tested as a radiotracer by Abass Alavi in 1976 at the University of Pennsylvania on volunteers. Positron tomography came along later. Cancer cells consume glucose faster than normal cells so the 18F will tend to accumulate to a slightly greater extent and reveal their position by positron annihilation. The two 511 keV x-rays simultaneously detected at 180o apart are identified by a ring coincidence detector. A single detection event is discarded.

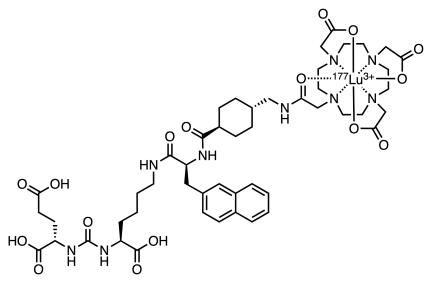
A radioligand that received FDA approval the same day as Pluvicto was Locametz or Gallium (68Ga) gozetotide. This gallium radioligand targets PSMA as does Pluvicto but is only a PET diagnostic agent.
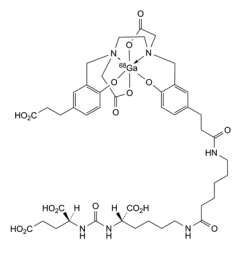
Locametz has 4 carboxylic acid groups, a urea group and two amide groups aiding water solubility and numerous sites for hydrogen bonding of this radioligand to the receptor. The organic portion of the Locametz is called gozetotide, named “acyclic radiometal chelator N,N’-bis [2-hydroxy-5-(carboxyethyl)-benzyl] ethylenediamine-N,N’-diacetic acid (HBED-CC).” The 68Ga (3+) cation is shown within an octahedral complex with a single hexadentate ligand wrapping around it. The short 68 minute half-life of 68Ga requires that a nuclear pharmacy be nearby to prepare it. The short half-life of 68Ga or other positron emitters as well as the possibility of destructive radiolysis to the ligand prevents preparing a large batch and stocking it. Locametz must be synthesized and transported prior to use. This rules out remote or rural hospitals.
Nuclear Chemistry
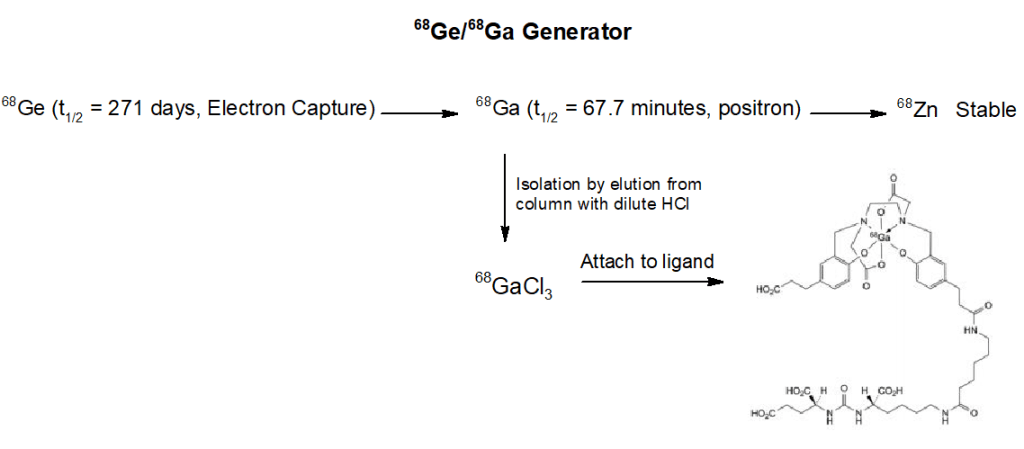
So, where does one obtain 68Gallium? Well, there are several methods out there. 68Ge/68Ga generators are produced commercially. One company is GeGantTM who offers 1-4 GBq of 68Ga. (Note: 1 GBq is 1,000,000,000 disintegrations per second).
From the scheme above we see the workings of a 68Ga generator. The ligand attachment is performed exterior to the generator. Atomic nuclei that are neutron deficient like 68Germanium can transform a proton to a neutron. There are two ways this can happen. In Electron Capture (EC) an inner “s” electron can be absorbed by a proton converting it to a neutron and emitting a neutrino by the weak nuclear force. This lowers the atomic number by 1, in this case 6832Germanium becomes 6831Gallium. The other mechanism is for the nucleus to emit a positron (anti-electron) and eject 1 positive charge as a positron (and an antineutrino) from the nucleus, resulting in a new neutron. The atomic weight remains constant, but the atomic number drops by one. If available energy in the nucleus is less than about 1 MeV, an electron capture is more favorable than positron emission.
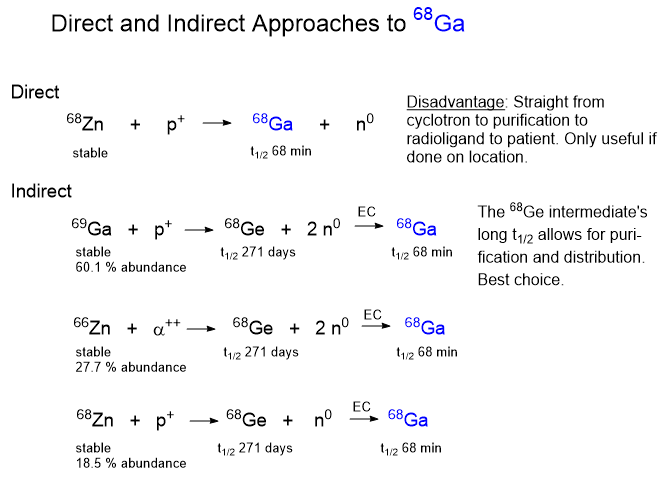
Once you know about the 68Ge electron capture reaction leading to the 68Ga isotope you have to ask, where does the 68Germanium come from? There are a few different ways to make and concentrate 68Ge and the method you use depends on the equipment available to you. One way is to accelerate protons to a high energy in a cyclotron and slam them into atoms heavier than germanium, such as rubidium or molybdenum. The collision with break the target nuclei into pieces by a process called “spallation“.
Cyclotrons
The first cyclotron was independently invented by Ernest Lawrence 1929-1930 at UC Berkeley. It was the first cyclic particle accelerator built. The idea of the cyclic accelerator was first conceived by German physicist Max Steenbeck in 1927. In 1928-1929 Hungarian physicist Leo Szilard filed patent applications for a linear accelerator, cyclotron, and the betatron for accelerating electrons. Unfortunately for both Steenbeck and Szilard, their ideas were never published or patented so word of the ideas were never made public.
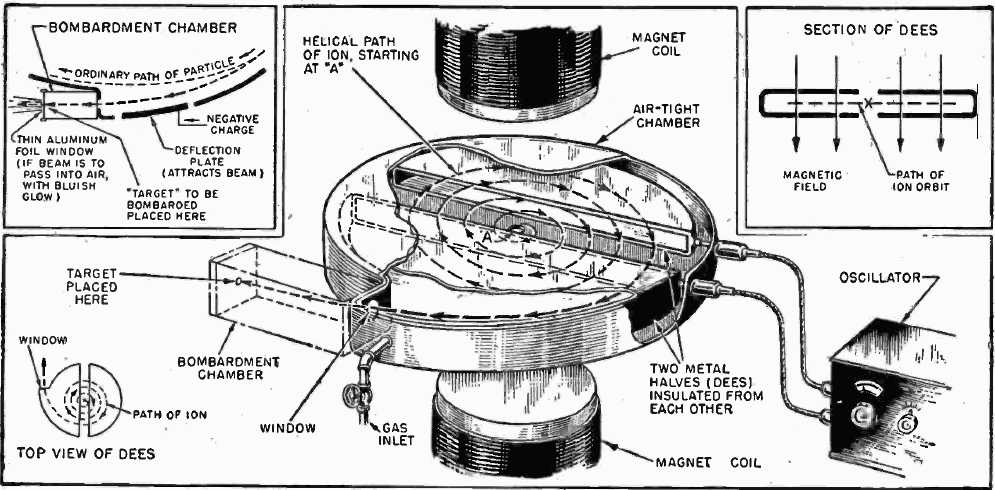
Where does one go to get a cyclotron? One company is Best Cyclotron Systems. If you are not sure of how a cyclotron works, check out the image below from Wikipedia. Note: A cyclotron can only accelerate charged particles like protons, electrons, deuterons and alpha particles which are introduced into the middle of the machine. A key component is the “D” or Dee, so-called because of their D-shape. The cyclotron has two hollow, coplanar Dees which are each connected to a high voltage radiofrequency generator. The Dees are open chamber-shaped electrodes that alternately cycle through positive and negative high voltage attracting and repelling charged particles under the influence of a powerful magnet. Because charged particles change their trajectory under the influence of a magnetic field, the particles follow a curved path of increasing diameter, accelerating until they exit the Dees and careen into the target.